Cataphasia (schizophasia)
Update : July 2016
Psychiatrists have often heard of Kraepelin's schizophasia, but it is only the excited pole of the same phenotype: cataphasia. As the ICD and the DSM did not retained language disorder as a significant symptom in psychosis (see historical) cataphasia is believed to be very rare since psychiatrist only consider the most severe clinical picture. Yet this phenotype is far from being uncommon, since it affects approximately 7-9% of hospitalized patients.
For the WKL school, cataphasia is a non-systematised schizophrenia. "Schizophrenia" means that the disorder comes with residual symptoms and "non-systematized" that it is not restricted to a single neurological system. In cataphasia, the residual symptoms mostly affect thought and language.
Cataphasia classically has a relapsing-progressive course. In most cases, patients are affected by acute episodes of bipolar characteristics as they could be dominated by thought excitation or inhibition. The episodes are interspersed with periods of clinical improvement. Patients may almost remit completely after the first episode, but the cognitive residual symptoms become more and more disabling with the recurrence of relapses. It is a phenotype with a very significant heritability.
Background
The "excited" pole of this phenotype has been described by Kraepelin under the term "schizophasia" (1908-1915). He already ascertained that this clinical picture had an unfavourable evolution in the long term, hence its classification among the "dementia praecox". The bipolar nature of the phenotype was described by Leonhard and his student Otremba in 1961, with a replication in 1963. They described this inhibited pole, as "poor in speech". It seems that this description has mainly been performed in the families with a schizophasic propositus having affected relatives with though inhibition. This is undoubtedly one of the finest illustrations of the familial aggregation principle as the bipolar nature of the phenotype is not systematically noticeable in a single subject.
The clinical picture of typical schizophasia (or "word salad") is rare. Thus, language disorders were not only excluded from the diagnostic criteria, but were also excluded from symptom scales of psychotic and mood disorders. As a result, psychiatrists trained with ICD or DSM generally not even notice these symptoms. Yet they persist between episodes, even if they are more discreet then. Several factors may have contributed to the overlooking of "fine" language disorder in psychosis:
- They are difficult to ascertain in migrant populations that do not share the same mother tongue as the host country. The population mixing and / or sub-crops in some developed countries like the US make them difficult to screen.
- If the type of language's abnormalities seems consistent between European languages, their salience might be variable in contrast. It is perhaps not so surprising that the initial observations have been made in German. German has features like its mode of word-construction and rigor in its grammatical constructions that make cataphasia anomalies particularly salient. For example, as new words are constructed by the mere concatenation of elementary words, the substitution of a verbal paraphasia to one of the elementary word is a neologism in German, though most salient as a mere verbal paraphasia (word approximation) which is more frequent in French (and probably in English as well).
- The role of antipsychotics is more difficult to estimate. If they can make schizophasia less obvious by merely calming down the excitement. However they have no effect on language disorders as such.
This was to stress why language and / or context have made the use of these symptoms difficult to generalize, thus explaining the relative disappearance of the interest in schizophasia / cataphasia.
Clinical features
The disorder predominantly affects thought and language. All the features typically attributed to the schizophrenic thought can be observed: logorrhoea without pressure of speech, distractibility of speech, contaminations, clang associations, loosening of associations, derailment, unrelated answers and incoherence, for the excited pole and alogia (poverty of speech) for the inhibited pole. But what is most characteristic is the addition of a specific language disorder to the disorganisation of speech: syntactical abnormalities (grammatical errors in the construction of sentences) and lexical errors (word approximation and verbal paraphasia, e.g. "I take care of a sizable fund with 600 to 900 workers to sort out", or neologisms formed by the mere juxtaposition of morphemes repecting the rules of the language, e.g. "We arrived like arrivors"). Errors are typically unstable and should not be confused with technical neologism.
The phenotype typically has a progressive remitting course (80-90% of cases). Pure progressive courses are rare (<5%). The remaining cases have a single identifiable episode (mostly of the inhibited pole), resulting in a severe residual state such that recurrences look like symptomatic fluctuations.
The polarity of an episode is defined by the excitation or the inhibition of thought process, and has nothing to do with mood or psychomotility.
Using ICD/DSM approach, episodes can be regarded as affective and/or psychotic. During inhibited episodes, an anxious but also a depressive mood can be observed. During thought excitation, both anxiety and ecstasy are possible. Conversely, psychosis can be in the forefront and may even have a paranoid tone up to the one seen in affective paraphrenia. All gradations are possible between purely affective and purely psychotic manifestations, i.e. schizo-affective episodes, but the thought and language component is constant and mandatory for the diagnosis.
Beside excited and inhibited episodes, mixed ones are not to be forgotten (22%). They combine both signs of thought excitation and inhibition. Although cataphasia is a bipolar phenotype, up to 50% of the patients may always have relapses of the same polarity, i.e. about 20% only have exited episodes (schizophasia), 30% only though inhibition. However it is rare that the other pole is not expressed in an affected relative. Between episodes, the patient is in partial remission in the sense that affective or psychotic dominance usually disappears (at least after the first few episodes) and the disorganization of thought and language steps back but still present.
- Episodes with thought excitation (Schizophasia) (35%)
The excitement of thinking manifests itself mainly by a talkativeness up to a logorrhoea generally without pressure of speech, i.e. in contradistinction with manic episodes of MDP. Prosody is often poor and flat, and the patients do not speak particularly loudly. These patients are often willing to talk and fill the time left free in an interview. The disorganization of thought and language is such that it is sometimes almost impossible to understand the meaning. In the most serious cases it can sounds like a "word salad" (schizophasia). But generally the disorder is less severe and a "psychological experimental test" (PET) is essential to carry out in order to reveal these anomalies. The absence of thought and language distortion during an acute exited phase is a good argument to exclude this diagnosis. Conversely the persistence of such anomalies should be ascertain in the residual state to confirm the diagnosis (see below).
In spite of the severe confusion of their thoughts, patients with cataphasia can carry out simple tasks independently (autonomous). They usually answer questions about their daily activity correctly, as well as other questions concerning concrete and/or familiar topics. But by their next sentence they may once again fallen into complete incomprehensibility especially when dealing with novelty.
Manic and / or anxious mood is more or less pronounced, and psychotic symptoms are often present. Hallucinations are rarely in the forefront. Delusions, more or less consistent with the patient’s mood is frequent. The psychomotility is animated and natural.
- Episodes with thought inhibition (poverty of words) (43%)
Thought inhibition is sometimes so extreme that no response can be elicited, the patient is mute. It is then impossible to examine the thought processes. In these cases, it is clear from the patient’s dazed facial expression that they either not paying attention to their environment or do not understand what is happening around them or what is asked of them. They should be distinguished from patients with catatonia because they do not have psychomotor symptoms: there is nothing remarkable about their behaviour and their movements are normal if somewhat slowed down. This slowdown predominates on voluntary movements and not expressive and responsive motility. In cases when the patient does still speak, there is significantly reduced expression, especially spontaneous expression, in terms of both quantity and content, i.e. alogia. A PET should bring out paraphasias and neologisms. Conceptual disorganization is often obvious but probably due to a loss of verbal output, thought disorganization might not be easily objectified. As stated previously, residual thought and language impairment has to be ascertained in the residual state to confirm the diagnosis.
Patients are generally more anxious than depressed. Delusions are frequent, mostly of the persecutory type, although poorly active due to thought inhibition.
- Mixed episodes (22%)
Elements of both poles are present without dominance of one over the other. There are no verbal excess nor alogia or both may alternate. Thought and language disorganization is in the forefront.
- Residual state
The residual cognitive disorganization that is the distinct attribute of this phenotype worsens with relapses. In this regard, episodes with thought inhibition are especially detrimental. Residual symptoms account for a severe handicap often responsible for vocational impairment especially in professions requiring adaptive abilities. However thought and language peculiarities are often missed during a standard interviewing especially after the first and second relapse. The psychological experimental test (PET) can unravel them. However, in its the classical form, PET sensitivity is 65% (n = 31) in the residual phase considering typical results only (at least a sufficient amount of 2 over 3 types of errors: logical, syntactic or semantic), 96 % when considering doubtful results (only one type of error, or small amount of errors). Moreover PET specificity appeared also poor as in a control population of patients hospitalized in an orthopedics ward, 17% (n = 72) had typical results, and up to 45% doubtful results. Sensitivity and specificity of the PET has not been studied vs. another psychotic phenotype during the residual phase.
An operationalized version of this test, the psychological experimental test operationalized for cataphasia (PET-OC) has been designed. By now there is only a French version which is currently assessed. First results were encouraging with a sensitivity and a specificity of 100% not only against normal controls (n = 26), but also against another form of endogenous psychosis (periodic catatonia, n = 14). But the number of cataphasic patients remains too poor to conclude (n = 8) (see O. Mainberger thesis).
Cognitive and above all, memory complains are frequent, although never concern thought and language. Neuropsychological testing usually shows a sparing of memory trace (Free and Cued Selective Reminding Test with Immediate Recall - FCSRT-IR). The decrement in the continuous performance test argues for a disorder of attention.
With the recurrence of episodes an affective flattening will set in (non specific).
When psychotic symptoms are present during the episode, they may persist for a while after the acute phase (acoustic-verbal hallucinations, persecutory ideation ...). These residual symptoms are non specific but may become more and more enduring with each recurrence.
Differential diagnosis
Confusional psychosis is relevant to differentiate from cataphasia because of its distinct prognosis. There are cases where the diagnosis is difficult to ascertain. This is especially the case during an episode with major thought inhibition because the verbal material can then be insufficient. During episodes with thought excitation the diagnosis requires to analyze the disorganization. By no way the differential diagnosis should consider the overall severity of disorganization. Indeed "incoherence of thematic choice", the typical feature of confusional psychosis can reach severe disorganization with excitation. As conceptual disorganization is evaluated from the verbal output it may not be possible to asses it selectively. Keys to the differential diagnosis are the syntactic and lexical disorders which are specific to cataphasia. When doubt remains, a psychological experimental test (PET) should be (re)done some time after the episode. As a moderate loosening of association can be part of the accentuated personality traits of confusional psychosis, conceptual and language disorder should be considered first for the differential diagnosis. The value of PET-OC remains to be assessed in this condition. Last, poor insight supports cataphasia.
In excited phases, periodic catatonia may also shows up speech disorganization. Priority should be given then to psychomotor symptoms: akinesia, hyperkinesia preferentially affecting reactive and expressive motility, parakinesia and stereotypy. Speech disorganization is there the pendant of psychomotor disorganization. Typically patients make short sentences which grammatical construction can be simplified up to become agrammatic ("telegraphic speech", tense, number, and gender errors...). This differs from the more elaborate but paragrammatic sentence construction in cataphasia. Moreover, in periodic catatonia, there is no lexical disorder other than what would result from perseverative or stereotyped speech. In inhibited phase, stereotypies are not sufficient to drive a periodic catatonia diagnosis. In fact they can also be a release phenomenon due to the severe thought inhibition. But parakinesias, predominance of inhibition on reactive and expressive motility explaining the lack of facial expression are indicative of periodic catatonia. In cataphasia, volitional motility is more severely affected, while expressive motility is preserve as indicated by the perplexed facial expression in thought inhibition.
Initially, the differential diagnosis with affective paraphrenia can be tricky as paranoid manifestations can be in the forefront. Conversely during acute episodes, affective paraphrenia may have some degree of thought disorganization. But delusions are less well organized and more changeable in cataphasia because of thought disorders. Again it is the assessment of PET during the residual state that should remove doubts.
The differential diagnosis with MDP is far from trivial. Cataphasic episodes are frequently diagnosed as manic or depressive episodes as defined by the IDC / DSM. Interestingly enough, psychiatrists trained with current diagnostic manuals are surprisingly poor in detecting disorganized speech and language during mood episodes when these are not accompanied by a paranoid (psychotic) component. This contrasts with psychiatrists trained in the former countries of the Eastern Bloc who immigrated in France. Despite the fact that they assess patients in their non-native language they are very attentive to this component and identify it as a risk factor for a schizophrenic course.
The disentangling between excited cataphasia and mania requires to be attentive to the kind of disorganization: related to the racing of thoughts (tachypsychia) in mania, whereas it remains present even in the absence of pressure of speech in cataphasia. Moreover typical lexical and syntactical errors are present in the later. During inhibited phase, it is not uncommon to diagnose cataphasic patients as depressive (uni- or bipolar) mainly on their dim behavior. Sometimes patients do not even complain of sadness or loss of pleasure when asked for. But even if one or the other would be present, language and conceptual disorganization should allow the differential diagnosis. The loosening of association is less characteristic as it can be observed in pseudo-confusional forms of MDP. Finally a PET (re)done at distance from the episode could help comforting the diagnosis.
The combination of thought and language disorders is not pathognomonic of cataphasia. There is only one other rare phenotype where this association can be seen: incoherent paraphrenia. The latter begins with a 1-5 years of process phase which ends up with the enduring residual clinical picture. Whereas speech and language are affected, incoherent paraphrenia is dominated by delusions and hallucinations. The hallucinatory experience is multimodal and pervasive. Patients' attention is captured by their inner world as evidenced by the emptiness of their gaze and their lack of facial expression. Patients overtly speak with their voices, which is never seen or only very transiently in cataphasia.
Proposed criteria
Introductory remarks
We have no doubt that classical WKL diagnosis is exceeding the operational criteria we propose here. Their main purpose is to allow a way to replicate these results among different research groups, a requirement for scientific objectivity. Indeed, it is unlikely that in the current competing context, clinicians and researchers will take the one to four years necessary for a clinician to be able to make reliable WKL diagnosis.
Because negative results might be mostly due to heterogeneity in the patient’s group, these criteria favor specificity over sensitivity. Accordingly, they do not account for the full spectrum of cataphasia, and some genuine cataphasic patients might not be diagnosed as such using them. As an example, the requirement for a relapsing-progressive course is just an easy way to limit the risk of including other phenotypes, mostly system schizophrenia, even though this criterion will be only filled by 80% of cataphasic patients. Thus, they are not adapted for epidemiologic or genetic research which should keep on with the classical WKL approach.
These criteria remain work in progress. Especially, they have not been validated in other groups than ours, and as such, we cannot guaranty that they will work as well for non-WKL trained investigators.
These criteria are inspired from those put forward by the Würzburg school, those of Sigmund and DRC Budapest-Nashville. Although the specific language distortions are well characterized in German and French, they might have to be refined in English and other language.
Finally, as this study was not concerning epidemiology, heredity or genetics, we also included the family aggregation principle as a minor criterion.
 Click here to see the present state of the wiki page. Only members are allowed to directly modify the criteria but we encourage any contribution (send a mail).
Click here to see the present state of the wiki page. Only members are allowed to directly modify the criteria but we encourage any contribution (send a mail).
Using the criteria
The background idea is simply to combine typical symptoms, i.e. qualitative disturbance of thought and language, with a typical course, i.e. of relapsing-progressive type. Since the former is rarely reported in ICD / DSM oriented case-notes, the criteria require prospective observation. When symptoms are too poorly characteristic, a cataphasic first-degree relative is required. Here are the different scenarios:
- Previous episodes are compatible + Observed episode with typical symptoms + Observed remission with typical OR non-typical residuals symptoms.
- Previous episodes are compatible + Observed remission with typical residual symptoms ± Observed episode with non-typical symptoms.
- Previous episodes are compatible + Observed episode with non-typical symptoms + Observed remission with non-typical residual symptoms + affected first degree relative.
Compatible previous episode(s)
For patients with a(many) previous episode(s) that was(were) not observed with the WKL classification in mind, the compatibility of previous episode(s) shall be assured.
Inclusion criteria
The following ICD diagnosis are compatible:
- Affective psychosis (anxiety, depression, mania or other kind of bipolar episode), no necessary psychotic feature.
- Psychotic episode of any kind except purely delusional.
Exclusion criteria
At least one episode not secondary to:
- Drug use or withdrawal.
- A general medical condition.
- A severe stressor, i.e. no reactive psychosis.
Observed episode with non-typical symptoms
Must be prospectively collected or retrospectively assessed on videotaped interview as it is very unlikely that ICD / DSM oriented case-notes can be helpful. The current episode can fulfill any of the ICD diagnosis criteria mentioned in the “compatible episode” section.
Criteria for the inhibited phase
At least, two items present during a sufficient amount of time:
- Extreme slowing of thought and speech up to mutism.
- Slowness predominating on movements requiring reflection relative to reactive and expressive movements.
- Patient’s facial expression is dazed (hebetude), reflecting his inability to figure what is going on around him.
Criteria for the excited phase (schizophasia)
Both criteria must be present (logical AND) at least during a significant amount of time:
- Logorrhea without pressure of speech (fill silences, no affectively driven pressure of speech).
- Various forms of disorganized speech (discourse): looseness of associations, derailments, digressions.
Exclusion criteria
Not secondary to:
- Drug use or withdrawal.
- A general medical condition.
- A severe stressor, i.e. no reactive psychosis.
Observed episode with typical symptoms (core symptoms)
Must fulfill the “Observed episode with non-typical symptoms” and at least two of the following criteria, prospectively assessed by the psychic experimental test:
- Syntactic disorders, i.e. paragrammatic sentences.
- Lexical disorders, i.e. word approximation, paraphasic errors up to neologism.
- Logical disorder and / or conceptual confusion, i.e. a special form of inability to converge toward the distinction between two concepts, e.g. difference between a child and a dwarf, between a river and a lake.
Observed residual state
Although full or nearly full recovery can be observed after the first episode, residual symptoms should be present in case of > 2 relapses, either typical or non-typical.
Exclusion criteria (out of the episode)
- Staring in the middle position or true catatonic symptoms according to WKL, i.e. parakinesia, true negativism (i.e. with ambitendance), waxy flexibility (with posture maintenance) ...
- Systematized chronic paranoiac delusion with a designated persecutor OR a delusion purely connected to affect/passion, i.e. erotomania, jealousy.
- Grossly disorganized behavior, i.e. there should be a striking difference between speech disorganization and the ability of the patient to behave rather normally in a familiar environment.
Observed residual state with typical symptoms (core symptoms)
- Should not have exclusion criteria for “observed residual state” + at least two of these symptoms:
- Syntactic disorders, i.e. paragrammatic sentences.
- Lexical disorders, i.e. word approximation, paraphasic errors up to neologism.
Logical disorder and / or conceptual confusion, i.e. a special form of inability to converge toward the distinction between two concepts, e.g. difference between a child and a dwarf, between a river and a lake.
Residual state with non-typical symptoms and an affected first-degree relative
Should not have exclusion criteria for “observed residual state” + one of these symptoms:
- Various forms of disorganized speech (discourse): looseness of associations, derailments, digressions.
- Incomplete insight.
+ An affected first-degree relative.
Etiopathogenic hypothesis
According to Leonhard, cataphasia is a non-systemized form of schizophrenia. In his mind this meant that multiple "neurological systems" would be involved in contradistinction to the systematized forms in which only one such system was supposed to be involved. He wasn’t thinking about a degeneration of one processing system but hypothesized that a regulatory system could be involved.
Aetiology
The pathology is unquestionably heritable with 15 to 25% of affected first-degree relatives, a figure that rises to 36% if parents with speech abnormalities but without ever having any affective or psychotic disorders are included. To date, no genetic analysis has been conducted on this phenotype. It must be said that patients’ residual mistrust during the free interval makes them reluctant to participate in the studies.
Pathophysiology
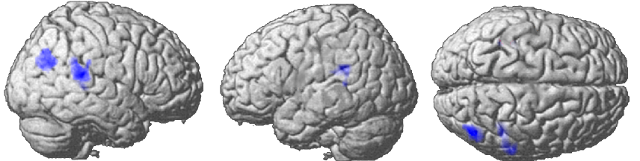
The core symptoms of cataphasia evoke the involvement of the language areas. This is exactly what has been showed by the analysis of the functional data of an ongoing study (Connect C3 - NCT02868879). Patients suffering from cataphasia were not only compared to controls, but also to other patients suffering from another psychotic phenotype (periodic catatonia) and thus also treated with antipsychotics. Cataphasic patients had a reduced activity in their temporoparietal junctions bilaterally (in blue, figure below). In addition, these regions showed a reduction in their functional connectivity with all peri-cingular areas, starting with the Broca area and its right-sided equivalent.
Clinical examples
Example of thought and speech disoders in a letter: Kajy.
References
Reference texts and additional material for cataphasia
- Kraepelin E. (1913) "Psychiatrie. Ein Lehrbuch für Studierende und Ärzte" III. Band. Klinische Psychiatrie". II. Teil, 8th ed. Leipzig: Johann Abrosius Barth p. 859-862.
- Kleist K. (1987) "Alogical thought disorder: an organic manifestation of the schizophrenic psychological deficit". In The Clinical Roots of the Schizophrenia Concept, ed. J. Cutting and M. Shepherd. Cambridge: Cambridge University Press. Translated from "Zur hirnpathologischen Auffassung der schizophrenen Grundstörungen. Die alogische Denkstörung". Schweizer Archiv für Neurologie und Psychiatrie, 1930:26, 99–102.
- Leonhard K. (2004) "Classification of endogeneous psychosis", ed. 1999. p. 95-104 (see English version). Translated from "Aufteilung der endogenen Psychosen", ed. 2004. p. 99-109 (see German version). Also translated in French "Classification des psychoses endogènes", in progress (see French version) and in spanish "Clasificación de las psicosis endógenas", ed. 1999. (see Spanish version) (cf. livre).
- Leonhard K. (1991) Extract from "Differenzierte Diagnostik der endogenen Psychosen", ed. 1991. p. 28-30 (see German version). Translated in French "Diagnostic différentiel des psychoses endogènes", ed. 2014. p. 37-40. (see French version) (cf. livre).
- Jabs B. "Untersuchungen zur Nosologie der Kataphasie". Habilitationsschrift defended in 2005 in Würzburg (German version only).
- Binder F. "Formale Denkstörungen in der Normalbevölkerung: Prävalenz und Vergleich zu Angehörigen von Patienten mit Kataphasie" Medical doctoral thesis defended the 16th of october 2009 in Würzburg (German version only).
- Foucher J. (2009) "35 psychoses", ed. 2009. p. 134-139 (French version only) (cf. livre).
- Mainberger O. (2015) "Validation du test psychique expérimental pour le diagnostic de la cataphasie" (Validation of the psychological experimental test operationnalized for cataphasia). Medical doctoral thesis defended the 30th of october 2015 in Strasbourg (French version only)
- The psychological experimental test operationnalized for cataphasia (PET-OC)
Selected articles
- Foucher JR, Zhang YF, Roser MM, Lamy J, De Sousa PL, Weibel S, Vidailhet P, Mainberger O, Berna F. (2018) A Double Dissociation Between Two Psychotic Phenotypes: Periodic Catatonia and Cataphasia. Progress in Neuropsychopharmacology and Biological Psychiatry (article, supplement1, supplement2) (doi) (Video presentation).
